


Stay tuned and follow the latest developments and news in Molecular Oncology.

Another important study by the Genekor Scientific Team on “Next Generation Sequencing (NGS) for the identification of PARP inhibitors’ predictive biomarkers” was presented by Dr. Floros Ir. Theofanis (Oncologist Pathologist, Military Doctor P.N. – Director, 5th Oncology Clinic of Metropolitan General Hospital) at ESMO CONGRESS 2022 in the form of a Poster.
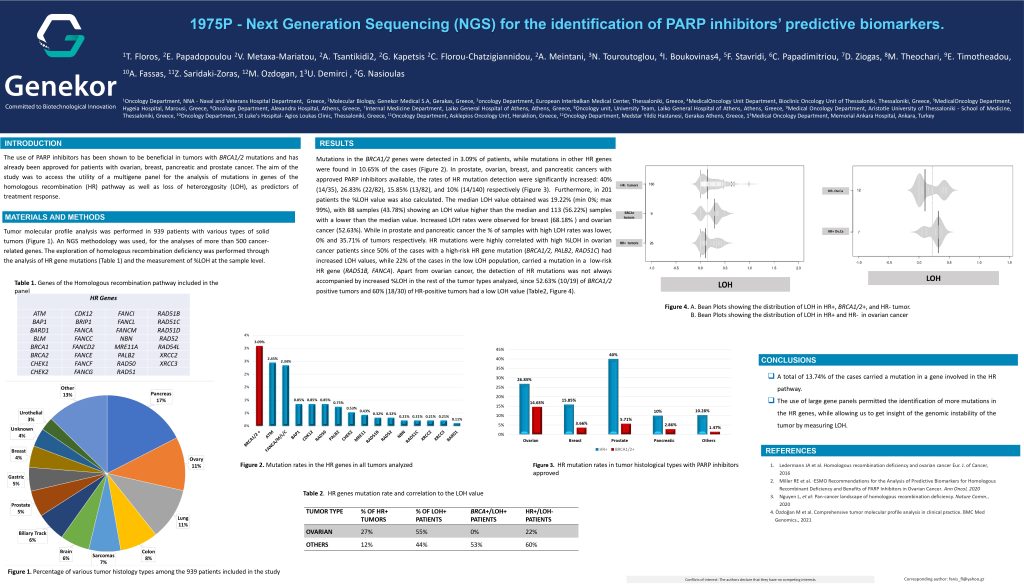
The use of PARP inhibitors has been shown to be beneficial in tumors with BRCA1/2 mutations and has already been approved for patients with ovarian, breast, pancreatic and prostate cancer. The study aimed to access the utility of a multigene panel for the analysis of mutations in genes of the homologous recombination (HR) pathway as well as loss of heterozygosity (LOH), as predictors of treatment response.
Mutations in the BRCA1/2 genes were detected in 3.09% of patients, while mutations in other HR genes were found in 10.65% of the cases. In prostate, ovarian, breast, and pancreatic cancers with approved PARP inhibitors available, the rates of HR mutation detection were significantly increased: 40% (14/35), 26.83% (22/82), 15.85% (13/82), and 10% (14/140) respectively.
Furthermore, in 201 patients the %LOH value was also calculated. The median LOH value obtained was 19.22% (min 0%; max 99%), with 88 samples (43.78%) showing an LOH value higher than the median and 113 (56.22%) samples with a lower than the median value. Increased LOH rates were observed for breast (68.18% ) and ovarian cancer (52.63%). In prostate and pancreatic cancer the % of samples with high LOH rates was lower, 0% and 35.71% of tumors respectively. HR mutations were highly correlated with high %LOH in ovarian cancer patients since 50% of the cases with a high-risk HR gene mutation (BRCA1/2, PALB2, RAD51C) had increased LOH values, while 22% of the cases in the low LOH population, carried a mutation in a low-risk HR gene (RAD51B, FANCA). Apart from ovarian cancer, the detection of HR mutations was not always accompanied by increased %LOH in the rest of the tumor types analyzed, since 52.63% (10/19) of BRCA1/2 positive tumors and 60% (18/30) of HR-positive tumors had a low LOH value.